
Coronavirus by the numbers
The data reminds us that the most vulnerable will be disproportionately impacted by the pandemic

The data reminds us that the most vulnerable will be disproportionately impacted by the pandemic
COVID-19 is a powerful reminder of the world’s inequalities and how we are only as strong as our weakest health system.
The International Rescue Committee is closely monitoring the pandemic’s effects on the 40 countries in which we work.
The data is clear: while wealthy countries struggle to contain COVID-19, fragile and conflict-affected nations face overwhelming challenges, from inadequate health care infrastructures to an alarming lack of testing.
The pandemic will not end anywhere until it is beaten everywhere. Go inside the sobering data below, which confirms the urgent need to protect the most vulnerable.
The information we are gathering about the spread of the coronavirus in conflict-affected countries is alarming, but it may be just the tip of the iceberg.
Recent data compiled by the IRC on May 21 reveal significant shortfalls in COVID-19 testing. Yemen, with only 31 coronavirus tests for every million people, is not an outlier. When the data was collected, Nigeria had only 165 tests per million people, northeast Syria just 59.
These figures offer a stark comparison to rich countries like the U.S., with 38,394 tests per million as of May 21, and Germany, with 42,581.
Our new analysis of countries where we work - including Yemen, Chad & Northeast Syria - show some of the lowest numbers of #COVID19 tests per million. Urgent support is needed capture all information to understand this pandemic - & to beat it. Learn more: https://t.co/G0rADnpHQFpic.twitter.com/YDhOnD7kow
— IRC - International Rescue Committee (@RESCUEorg) May 22, 2020
The lack of testing means that the full scope of the outbreak in conflict-affected countries may be obscured, hindering efforts to trace, isolate and treat the disease.
With only 11 ventilators as of April 9, the West African nation of Burkina Faso is one of many countries facing a shortage of medical supplies exasperated by violence. Almost 500,000 of the country’s 20 million people have had to flee their homes as armed groups continue to consolidate their presence across swathes of the country.
"The major increase Burkina Faso has seen in attacks by armed groups over the past year compounds the difficulty of mitigating the spread of a disease in an active conflict area, as we've seen with Ebola in the Democratic Republic of Congo," says Bob Kitchen, IRC vice president of emergencies and humanitarian action.
Our new report reveals grave shortages of ventilators and ICU beds in fragile countries like Venezuela, South Sudan, Somalia. #COVID19 will hit countries in crisis the hardest – if we don’t act now. RT to help us raise awareness – and learn more here: https://t.co/mm5QLmlrrtpic.twitter.com/Oga93MisHq
— IRC - International Rescue Committee (@RESCUEorg) April 9, 2020
Other countries compromised by conflict include Syria, where there were 85 attacks on health facilities in the north of the country last year alone, and Yemen, where only half of the nation’s hospitals are fully functional.
These nations face a “double emergency” as the virus’s health effects are coupled with escalations in conflict and political and economic instability provoked by the outbreak.
Venezuela is suffering from a longstanding economic and humanitarian crisis that has rendered it ill-prepared to face the pandemic.
At least 4 million people have left the country seeking a better life. That number includes half of the country’s doctors; 90 percent of its hospitals are short of medicine and critical supplies.
In addition, Venezuelans living outside the country are affected disproportionately by lockdown measures in the region that make it impossible for them to earn an income. In Colombia, a near-shut-down of the border has left thousands attempting to return home stranded or forced to use unsafe routes.

Social distancing is one of the proven ways to slow the coronavirus. But refugees around the world face overcrowded conditions that make the life-saving strategy nearly impossible.
The now-infamous Diamond Princess cruise ship offers a measure of comparison: the virus spread four times faster on the ship than in Wuhan at the peak of city’s outbreak. This was partially due to the ship’s population density: the Diamond Princess housed 24 people for every 1,000 meters squared. Moria refugee camp in Greece has 204 people per 1,000 meters squared.
View this post on InstagramA post shared by International Rescue Committee (@rescueorg) on
Based on potential response scenarios, the IRC estimates between 500 million and up to 1 billion coronavirus infections, and between 1.7 million up to 3.2 million deaths, in 34 countries where we work—including war-torn nations like Afghanistan, Syria and Yemen—without context-appropriate and immediate action.
These numbers are conservative. The data presumes levels of medical care available in China (the source of the best available COVID-19 mortality figures) would be available elsewhere. But the fragile states in question have nowhere near the health care capacity of China.
“These numbers should serve as a wake-up call,” says IRC president and CEO David Miliband.
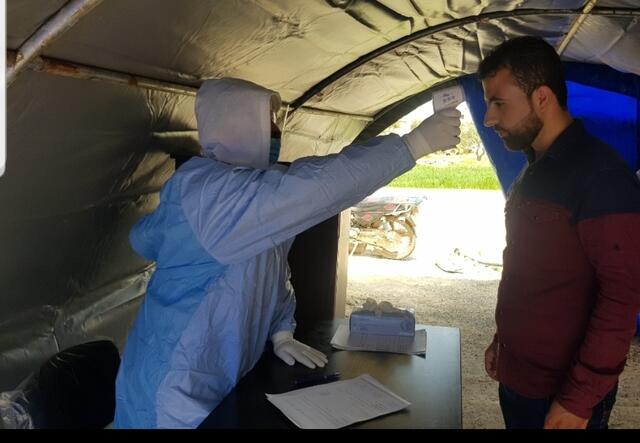
IRC teams on the ground are providing essential health care services, equipping aid workers with protective gear and delivering hygiene kits to people in refugee camps and crisis zones.
The IRC's response strategy aims to mitigate the spread of COVID-19 and treat patients while focusing on meeting the other health and economic needs of the people we serve, and expanding our protection services for women and girls. As part of this effort, our research and innovation team is helping create cost-effective COVID-19 solutions tailored for the crisis zones in which we work.
The IRC has launched a $30 million appeal to help us mitigate the spread of coronavirus among the world’s most vulnerable populations, protect our staff, and ensure the continuation of our lifesaving programming.
Donate now to support our work.